Glaucoma is the second leading cause of blindness in the world.
|
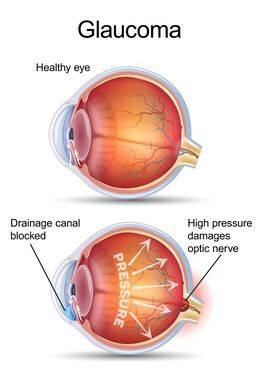
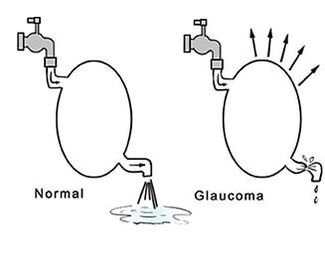
A simple definition of glaucoma is that the pressure (IOP) in your eye is too high for you. Over time, the elevated IOP kills the Retinal Ganglion Cells (RGC) and the nerves attached to them. The RGC and their nerves are responsible for sending what you see with the eye to your brain. Left untreated the pressure eventually kills the RGC and the nerves. Once the RGC and nerve “die” they are lost since no regeneration occurs. This results in a permanent loss of vision. The loss begins with your side vision and works it’s way to your central vision. |
Are you at Risk?
Glaucoma is more common than people think. In fact, it has been estimated that there are over 60 million case worldwide. Although Glaucoma is more often found in older adults, it can happen at any age. Your ethic background, family history, medications, and personal medical conditions, such as Diabetes and others may increase your risk. The physical structure of your eye also may increase your risk. A thin cornea, a large cup to disc ratio, and severe nearsighted are examples of physical structures that may increase your risk of having or developing glaucoma.
Types of Glaucoma:
|
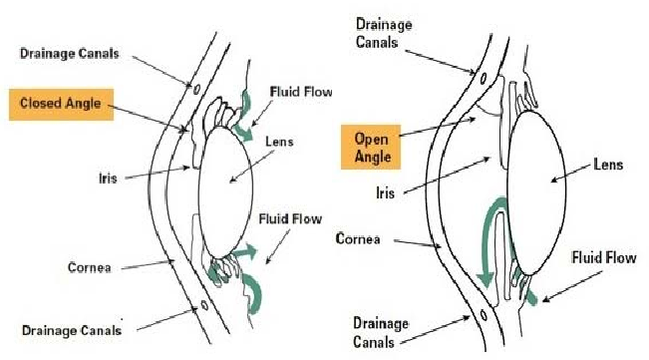
Open Angle is the most common form with it making up at least 90% of glaucoma cases. Open Angle glaucoma includes a
sub - category called Normal, or Low, Tension glaucoma. These patients have an IOP in the normal range but still exhibit damage due to the IOP being to high for them personally. A Secondary Glaucoma is due to trauma or as a side effect of some medications. Angle closure Glaucoma is rare but is considered a medical emergency. |
What testing can you expect if you are a suspect:
After reviewing your personal history, the doctor conducts an exam. There is no single test to diagnosis glaucoma. The single exception is if the IOP is > 30. The IOP is checked during your eye exam. The doctor also evaluates cup to disc (C/D) ratio of the optic nerve inside your eye. Your pupils are checked for potential abnormalities. Based on risk factors and exam findings, additional testing may be required. It may be helpful to think of a jigsaw puzzle to obtain a diagnosis of glaucoma.
Some possible test are:
- VEP checks the visual pathway from the eye to the brain. It may detect early glaucoma before any physical damage occurs.
- Pachometry checks the corneal thickness. Thin corneas indicate a higher risk for glaucoma.
- ERG checks retinal function. The RGC are damaged by glaucoma resulting in decreased retinal function.
- Gonioscopy determines if the eye angles are open or closed.
- OCT is used to determined physical damage to the RGC.
- Visual Fields measure your perceived visual loss. You will lose about 30% of the RGC before the loss is noticed.
- Serial IOP determines your average IOP.
I've been diagnosed with Glaucoma....now what?
Once a diagnosis of glaucoma is reached, you will be placed on medication. Eye drops are prescribed to lower the IOP. By lowering the IOP, the progression of glaucoma can be slowed or halted.
Like most chronic diseases, regular monitoring is done. For glaucoma a 12 week cycle is usually used. During these progress exams, your IOP will be check to ensure that it remains lowered. Additionally, one or two of the test used to diagnosis the disease will be repeated to watch for progression. If the pressure has been lowered but the testing shows progression of the disease then your medication may need to be adjusted or changed completely.
Additionally, over time, some patients will experience a return of elevated IOP as the body adjust to the medication. Without the regular progress exams, it is not possible to evaluate the effectiveness of the medication. Patients need to understand that refills for medication are dependent on your progress exams. Simply put, if the medication is no longer effective, a change is required. Using an ineffective medication allows the disease to progress as if no medication is being used.
With proper treatment and monitoring, glaucoma can be managed. The ultimate goal is to protect your vision during your lifetime.
Like most chronic diseases, regular monitoring is done. For glaucoma a 12 week cycle is usually used. During these progress exams, your IOP will be check to ensure that it remains lowered. Additionally, one or two of the test used to diagnosis the disease will be repeated to watch for progression. If the pressure has been lowered but the testing shows progression of the disease then your medication may need to be adjusted or changed completely.
Additionally, over time, some patients will experience a return of elevated IOP as the body adjust to the medication. Without the regular progress exams, it is not possible to evaluate the effectiveness of the medication. Patients need to understand that refills for medication are dependent on your progress exams. Simply put, if the medication is no longer effective, a change is required. Using an ineffective medication allows the disease to progress as if no medication is being used.
With proper treatment and monitoring, glaucoma can be managed. The ultimate goal is to protect your vision during your lifetime.